
How To Travel With Medications
The A to Z of
Travelling with Diabetes

Diabetes should not prevent you from having fun, from making a trip to an exotic country or a simple mountain hike. If you have diabetes and want to travel, you just need to carefully plan your trip. There are of course always unexpected events (lost luggage, plane delays etc), but if you are well prepared, you can usually overcome these difficulties quite easily.
“The real voyage of discovery consists not in seeking new landscapes but in having new eyes.“
Marcel Proust
“The real voyage of discovery consists not in seeking new landscapes but in having new eyes.“
Marcel Proust
There are many misconceptions about diabetes and insulin, and quite often the things that seem quite obvious to your doctor are a complete mystery to you.
This “A to Z of traveling with diabetes” was developed by MedActiv with a team of specialists and international medical consultants. We try to provide you with information that is factual and current.
If you have any comments, suggestions or questions about diabetes, please send us an email using our Contact Us form.
Advice

About the author
Uwe Diegel (born 1965 in New Zealand), is a specialist in various forms of medical diagnostics such as blood pressure, temperature, asthma and diabetes. He is the holder of several patents relating to temperature and blood pressure measurement.
After studying music in Canada and in South Africa, he performed worldwide as a concert pianist for several years. In 1989 he changed his career due to an injury to his right arm. In 1992 he entered the world of medical diagnostics, quickly developing a particular interest in cardiovascular diagnostics.
His intense scientic curiosity has led him not only to develop new technologies in this field, but also to interest himself in the field of medical manufacturing, industrial design and problems faced by Chinese manufacturing concerns.
Uwe lives in Paris, France, where he runs HealthWorks Global and does fundamental research in blood pressure diagnostics. He is today considered to be a foremost expert in the eld of blood pressure management and in the manufacturing of medical diagnostics devices.

Travelling with Diabetes
Before your trip
Talk to your travel agent
Tell your travel agent that you have diabetes and explain the specific requirements that the journey might entail. This way your trip can be tailor made to better meet your needs. A missed connection in an airport can ruin even the best prepared holidays.
Talk to your doctor
Consult with your doctor before planning or confirming your holidays. Discuss your itinerary with him and develop plans for meals and medication, especially when traveling through different time zones. Ask your doctor what to do in the eventuality of you becoming sick while on holiday.
Talk to your pharmacy
Ask for a list of all your medications (including generic names and dosages) from your pharmacist (especially oral medications for diabetes and insulin). If you take insulin, be familiar with the different types of insulin and know if your insulin is fast acting, intermediate or slow. Carry a copy of this list with you at all times.
Travel Insurance
Make sure you have comprehensive travel insurance to cover your trip, and keep copies of your insurance documents with you in case of an emergency. Some insurance plans do not cover pre-existing conditions, which may include diabetes. Make sure your diabetes is covered by your medical plan.
Diabetes in a foreign language
Learn how to say, “I have diabetes” and “orange juice or sugar, please” in the language or languages of the countries you visit. Try to find out what the important words for diabetes are (insulin, sugar, hypoglycemia, etc.) in the country where you travel in case you have a medical emergency or if you need to let people know that you suffer from diabetes.
Glucagon
If you use insulin to manage your diabetes, you should also ask your doctor if glucagon is suitable for you. Glucagon is given by injection and is used to treat severe hypoglycemia, a condition that can cause seizures or unconsciousness. If you are traveling in a remote area with no ambulance service, it is important that your traveling companion learn how to administer glucagon. Talk to your doctor if you are not familiar with its use.
Medications
Make sure you have enough medicine to cover the entire period of your trip. It may also be a good idea to double the amount of medication you need for your trip and to put one set in your hand luggage and the other in the hand luggage of your travel companion. That way you’ll have a backup if you happen to lose one of your bags during the trip. Keep your medications in properly labeled containers, as issued by your pharmacist, and keep your insulin at the right temperature (between 2 and 8°C). To transport your medication at the right temperature, use a MedActiv bag.
Your glucose levels will vary throughout the day, so it is important to keep an eye on them at all times
Boxes used for syringes / needles
In addition to your medication, you will need a secure box to dispose of your used needles. These boxes are usually available from your pharmacy. Talk to your pharmacist or your doctor about how to get one.
Vaccinations
Be sure to get the necessary vaccinations at least four weeks before your departure to allow time to deal with possible side effects.
Prescriptions and Diabetic Cards
Ask your doctor to give you a prescription in English, because English is the most widely understood language by doctors worldwide.
Travel certificate
Download a travel certificate and ask your doctor to complete it. This travel certificate says that you have diabetes and that you should not be separated from your medicine, and that this medicine should be stored at a temperature between 2 and 8°C. You can download a certificate from the MedActiv Australia website by clicking Here.
Sea sickness
If you suffer from seasickness, take some carbohydrates in liquid form (juice or soft drinks) with you.
Assistance
When booking, always inform your airline or your travel agent if you need assistance during the trip.
The journey itself
Copies of your prescriptions
Make copies of your prescriptions and keep them in your hand luggage in case customs or airport security ask you questions about the medications you are carrying.
Medication
Your glucose levels will vary throughout the day, so it is important to keep an eye on them at all times. Divide your medication and diabetes supplies in half and put one half in your carry-on bag and the other half in the baggage of your travel companion (if possible). Above all, make sure that you have some of your medication in your carry-on. Take extra supplies and medicines in case of loss or theft.


Include any other supplies you might need, including treatment for hypoglycemia, food, drinking water, walking shoes, sun cream and medication against nausea and diarrhea. Keep your insulin at the right temperature (between 2 and 8°C). To carry your insulin and glucagon at the right temperature, checkout our range of Travel Packs to see which pack will suit your needs.
Customs
- Inform the security guards that you have diabetes and that you are carrying medical supplies. Your medication must have a prescription label with your name on it.
- All medications must be labeled with the manufacturer’s name.
- Syringes are only allowed through security if you are carrying insulin

"I come from a family of diabetics, so am defined by my lifestyle. But with careful management and understanding, diabetes is now sorted…"
Uwe DIEGEL
Again, if you warn the security guards BEFORE they ask any questions, they will normally bend themselves backwards to help you. You’ll probably end up jumping the line and getting through before everyone else. However, if you are a jerk about it, you could end up getting that dreaded full cavity body search.
Customs and insulin pumps
Notify a security officer in advance if you are using an insulin pump. The walk-through metal detectors and hand-held metal detectors can affect the operation of an insulin pump, so if you are using an insulin pump you should ask the security agent for a manual search in a private area. You must inform them that your insulin pump cannot be removed.
Where to put your insulin on the plane
The luggage zones on a plane are all pressurized and maintained at a constant temperature of about 5°C. This is a standard for the vast majority of airlines. So it’s not a problem for you to put some insulin in the hold. Insulin is affected by extreme temperatures and should never be stored in a nonpressurized aircraft. It is important to inspect your insulin before each injection. If you notice anything unusual with the appearance of your insulin, immediately replace it with fresh insulin.
Generally, it is recommended never to leave your insulin and, if possible, to carry it as hand luggage, because if your insulin is in your main luggage in the hold and that your suitcase is lost, it may ruin your vacation. Wherever you go, always keep enough insulin for the duration of the trip and one day more. MedActiv manufactures a range of different isothermal products for the safe transport of insulin by plane.
Look for simple solutions
Tips for different types of travel
By plane
Be sure to give yourself extra time before your flight because when you arrive at the security check with insulin and syringes, the security control of the airport may take a few minutes more.
Airlines usually offer special meals for diabetics (however you must notify them at least 48 hours in advance), but with a little planning, the regular meals in an airplane can normally fit into your usual diet. Always have appropriate snacks with you in case your flight or the meal is delayed, or if the meal provided does not have enough carbohydrates. Be aware of time zone changes and of the timing of your meals and prepare your medication accordingly. If you sleep during your flight, use an alarm clock or ask the flight
attendant to wake you up at meal times or when it is time to take your medication.
Try to stay active during your trip and walk through the terminal before boarding, do simple stretching exercises in your seat or make circles with your ankles. If possible, elevate your legs every now and then.
If you are using a prescription drug it is important to have it with you and to know how to use it and any side effects that you may have. This will help you in explaining to the flight attendant how to help you if you need it.
By car
Whether you are a driver or a passenger, it is very important to check your blood sugar regularly. Check it before you leave home, and again every four hours during your trip.
Stop every few hours to stretch your legs and do some physical activity to improve circulation in your legs. At the first sign of hypoglycemia take a dose of simple sugars such as glucose tablets, 175 ml of fruit juice or even a soft drink. Follow this with longer acting carbohydrates and protein such as a sandwich. Do not start driving again until the symptoms have disappeared and your blood glucose values are greater than 6 mmol/l. If you take insulin, avoid driving between your injection and your next meal. Limit your driving to a maximum of 12 hours per day, or six hours between meals. Keep your medication, meals and snacks as regular as possible. If you are stuck in a traffic jam, car breakdown, or take wrong directions, it will not always be possible to find a restaurant or supermarket, so always bring along enough stuff to treat low blood sugar (glucose tablets, fruit juice or soft drinks).

Planes, trains and automobiles…
Boat
Cruise liners are known for their extravagant buffets. With such a wide variety of appetizers and dishes available, it is easy to overindulge. If possible, try to get a sample menu of the cruise and you’ll then have an idea of the types of food served and will be able to plan your meals accordingly.
Stay active to compensate for any extra food you eat. Cruise ships offer a wide range of activities; try an aerobics course, swimming, or just have a romantic stroll on the deck at sunset.
It’s always a good idea to make the cruise staff aware of your diabetes in case of problems.
Hiking
Hikes in the great outdoors are often the most fun but remember the cardinal rule: do not go camping or hiking alone. Tell someone where you are going and when you expect to return so that you can be found in the case of an emergency. Take a first aid kit and if you use insulin, talk to your doctor about it.
The key to enjoying a camping trip is to avoid things that will significantly change your glucose levels, such as higher levels of intense physical activity than usual. Watch out for cuts, bruises, sunburns, blisters and insect bites.
Make sure your food and water are not contaminated. Be sure to eat and drink enough to meet your needs - bring extra food, water, medication and sugar. If you are going to be very active, you may need to take less insulin, but talk to your doctor before doing so.
During the trip
Check your blood sugar during the trip
Checking your blood sugar while traveling is as important (if not more) than when you are at home. Bring the instruction manual for your meter, as well as extra batteries and test strips. To facilitate the monitoring of injections and meals during time zones changes, keep your watch to the departure time zone until the morning after your arrival.
Check your blood sugar as soon as possible after landing. With the time differences, it can be hard to tell if you have a very low or very high glucose levels.
After a long flight, try to relax for a few days to get your system back in shape. Check your blood sugar regularly. If you take insulin, plan your activities so that you can integrate your insulin and meals in your workflow.
Insulin during the trip
Insulins sometimes have different brands and dosages in some countries. If you need to buy insulin during your trip, make sure that the brands and insulin dosages are the same as those you normally use. Try using your own drugs and syringes in the third world countries and avoid using local needles if they are not sterile.
In general, you should use the brand and formulation of insulin that was prescribed by your doctor. However, if you need more insulin when you’re on the road and your usual brand is unavailable, you can replace your insulin by an equivalent formulation of another brand. However, any change in the formulation (ex. fast-acting for slow-release) requires medical supervision.
Time zone changes for insulin users
Long trips often cross several time zones, so a 24-hour day may be extended or shortened depending on your direction of travel. You should adjust your insulin schedule accordingly. Your glycemic control may be disturbed by a change in schedule, modi ed activity, or a disturbance in your sleep patterns.
Time zone changes for users of oral medications
If the time difference is less than three hours, you can move the time of your medications by an hour and a half. If the time difference is more than three hours, you should ask your doctor for advice.
- When traveling east, your travel days will be shorter. If you lose more than two hours, you will need to take less intermediate or slow insulin.
- When traveling west, your travel days will be longer. If you gain more than two hours, you will need to take extra units of insulin and more food.
- You can change the time of your meals and injections for up to two hours in a day without adjusting your insulin dose or your meal plan.
- Follow your usual meals whenever possible.
- If you cross more than two time zones, you should prepare a schedule of meals and insulin together with your doctor.
Emergency Food
Always carry some snacks with you in case of a drop in blood sugar or in case you are unable to eat your planned meal on time. Cheese, biscuits, fresh or dried fruit, energy bars and sandwiches are all healthy choices that are easy to carry in a handbag. Also carry some fast-acting sugar with you, such as glucose tablets or juice.Avoid tap water in developing countries. This includes ice cubes made from tap water.
Alcohol, diabetes and travel
Consumption of alcohol may increase your risk of hypoglycemia. However, travel is often equivalent to a holiday where alcohol consumption might be higher than usual. To reduce this risk, take the following steps:
Before drinking alcohol…
- Eat regular meals, take your medication and check your blood sugar frequently (keep your meter with you).
- Keep a treatment for hypoglycemia with you (glucose tablets or fruit juice).
- Wherever you are, make sure someone knows how to recognize signs and symptoms of hypoglycemia and how to treat it so that they can help you.
- Be aware that glucagon, a treatment for blood glucose, does not work when alcohol is in the body. For this reason, make sure someone knows how to call an ambulance if you lose consciousness.
- Wear diabetes identification such as a Diabetic Card or a Medicaid bracelet.

While drinking alcohol…
- Eat foods that are rich in carbohydrates.
- Eat even more foods that are rich in carbohydrates if you dance, play sports or do other unusual physical activities.
- Always mix your own drinks. Use less alcohol and stretch your drinks with sugar-free mixers.
- Drink slowly. Between each glass, have a drink without alcohol.
After drinking…
- Tell a responsible person that you’ve been drinking. They should watch for symptoms of hypoglycemia.
- Check your blood sugar before going to bed.
- Take a carbohydrate snack if your blood sugar is lower than usual.
- Set an alarm or ask a responsible person to wake you up at night and early in the morning - hypoglycemia can occur at any time for 24 hours after alcohol consumption.
- Get up on time the next day for any food, medication or insulin that you normally take. Skipping medication or insulin may cause hyperglycemia, ketones and DKA.
Diabetes and foot care during travel
Diabetics need to pay attention to their feet.
- Take at least two pairs of shoes in order to change shoes as often as possible. Changing shoes helps prevent blisters and painful pressure points.
- Take comfortable shoes and socks and a first aid kit to treat minor injuries to the feet.
- Do not walk barefoot. If you are in the sea or walking on the beach, wear shoes made especially for the ocean. Protect your feet at all times when you’re swimming in the ocean, walking on the beach or in a park.
- Do not wear open-toed shoes, including sandals, ip ops, or others (you increase your risk of injury and infection when your toes are exposed).
- Follow your normal daily care for your feet.
If you become ill while on holiday
When you are sick, your blood sugar levels can uctuate and be unpredictable. During periods of illness, it is VERY IMPORTANT to:
- Test your blood glucose every two to four hours.
- Continue taking your diabetes medication.
- Drink plenty of water or fluids without sugar. Avoid coffee, tea and sodas as they contain caffeine that will make you lose more fluids.
- Replace solid foods with liquids that contain sugar if you cannot eat your usual meals.
- Take at least 15 grams of carbohydrate every hour.
- Call your doctor or go to an emergency room if you vomit and/or have diarrhea twice or more in less than four hours.
- If you take insulin, continue taking
it while you are sick. Check with your doctor if you think that you need to adjust your insulin doses during your illness.
- Relax.
- If you have travel insurance, take your documents with you to hospital.
The storage and transport of insulin
Insulin must be stored properly, because it will quickly become less effective if it is exposed to extreme temperatures. At an ambient temperature of 25°C, insulin will retain its effectiveness for about three weeks. At a temperature of 28°C, insulin will lose about 14% of its efficiency over a period of one month, and at 32°C it will lose about 18% of its efficiency over the same period. If insulin is exposed to temperatures below 0°C or is frozen, it almost immediately develops crystals that make the injection dangerous and uncomfortable. The ideal storage temperature for insulin is between 2 and 8°C. At this temperature insulin can be maintained almost indefinitely.
Transporting your medications
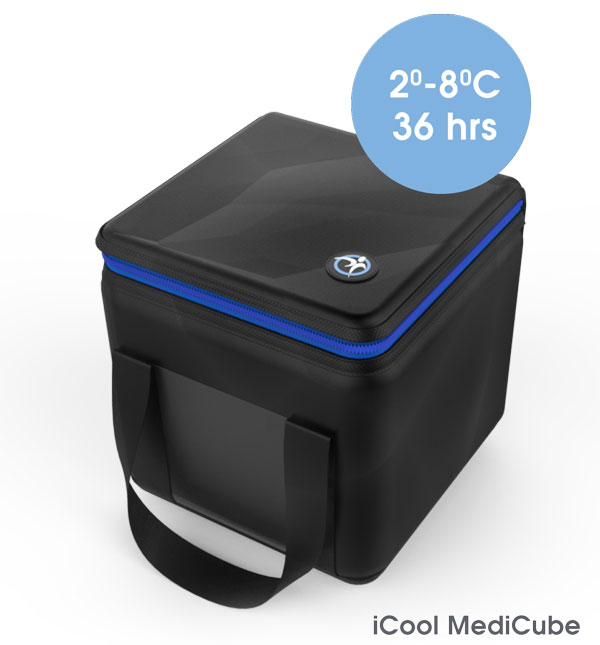
MedActiv has developed a range of cooler bags specially adapted to keep your insulin at the right temperature. These bags are divided in two main categories that are the EasyBag and iCool range.
EasyBag
- The EasyBag uses gel crystals that cool insulin when they are placed in contact with water. To activate the EasyBag, simply immerse it in water for 40 seconds. The crystals in the panels of the EasyBag change into a gel that stays fresh for about five days using an evaporation process that will keep insulin at a temperature between 16 and 25°C (up to an ambient temperature of 32°C). Insulin can be stored for up to three weeks at this temperature.iCool
- the ultimate expression of innovation at the service of technology - The iCool bags use a new generation of chemical ice packs that do not sweat and that have a slower thawing period than traditional ice packs. This allows people with diabetes to carry their insulin safely when traveling, at work or on vacation. The iCool bags keep insulin for up to 36 hours at 2 to 8°C and also include separate compartments to carry all your diabetes accessories (blood glucose meter, needles, bandages, etc.).Useful hints
- For environmental reasons, more and more hotels are using coded cards to open the doors of their rooms and these cards are also often used as a switch to turn on and off the electricity in the room. This means that when you leave your hotel room, you take your card with you and turn off all the electricity in your room (including the little bar fridge where you keep your medications cool). To work around this problem, just use any old plastic card (a gym membership card, business card, etc.) to switch on the power in your room. Leave it permanently in the room so that the electricity stays on.
- If you need to freeze the ice packs of your MedActiv travel bag before leaving the hotel, the refrigerators in the hotel rooms are generally not of a very good quality and will not completely freeze your ice packs. So instead of using the bar fridge in your room, go down to the hotel bar and ask the helpful staff to freeze them for you. After all, they always need ice in bars and therefore have high quality freezers.
Useful Sites
MedActiv (transport solutions for medications);
www.medactiv.com.au
Have diabetes, will travel…
About MedActiv
MedActiv is a global leader in the development of transport and storage solutions for sensitive medication. Our products are designed to give users the freedom to travel knowing that their medication is kept at exactly the right temperature. As the chosen partner of major pharmaceutical companies worldwide, MedActiv is constantly pushing back the boundaries of this industry.
The future is friendly
The MedActiv solutions are specially designed to bring added value to the medications they are made for. Strategically located in France, UK, USA, Australia, Tunisia and Taiwan, we have the reputation of always anticipating the needs of our customers with an approach that is based on the total satisfaction of the end-user of the medication.
Our team of experts includes physicians, patients and engineers who are dedicated to finding better solutions for the transport and storage of sensitive medication. Many of our products have been rewarded with industrial design prizes worldwide. The entire MedActiv range of products received the Handicap 2010 Award from the Mayor of Paris.
Exceeding your expectations for the transport and storage of medications
For Uwe DIEGEL, creator of MedActiv, the company represents a personal investment. “In 2003, my brother almost died following an incident where his medication was accidentally frozen in a hotel. So I started this company because of reasons that are more of a personal nature than just business. MedActiv is for me the ultimate expression of innovation at the service of healthcare. If the MedActiv products are so popular, it is because they are designed by patients for patients and because we speak directly with users of the medications to really understand their needs.“

Transporting your Insulin
An interview with Uwe DIEGEL on different methods for transporting insulin.
Click on the pic or here to see the interview.
ABOUT MEDACTIV
MedActiv is a global leader in the development of transport and storage solutions for sensitive medication. Our products are designed to give users the freedom to travel knowing that their medication is kept at exactly the right temperature. As the chosen partner of major pharmaceutical companies worldwide, MedActiv is constantly pushing back the boundaries of this industry.
MedActiv North America www.medactiv.ca MedActiv Europe www.medactiv.com MedActiv South America www.medactiv.cl MedActiv Australia www.medactiv.com.au
© 2023 Medactiv Australia - All rights reserved.
Unauthorised duplication or publication of any materials from this Site is expressly prohibited.
Unauthorised duplication or publication of any materials from this Site is expressly prohibited.


